Medicaid is a government-funded health insurance program designed to provide essential healthcare coverage to low-income individuals and families in the United States. It’s a joint effort between the federal government and individual states, which means that eligibility requirements and benefits can vary slightly from state to state.
While Medicaid can be a lifeline for many, it’s important to understand that there are specific criteria that must be met to qualify. These requirements typically involve factors such as income, assets, and other demographic information. If you’ve recently been denied Medicaid coverage, it’s essential to familiarize yourself with the program’s eligibility guidelines to determine your next steps.
Understanding the Eligibility Criteria Of Medicaid
Medicaid eligibility can vary from state to state, but the federal government provides some general guidelines. To qualify, you typically need to be a U.S. citizen or lawful permanent resident. One of the most important factors is your income, which is assessed based on the Modified Adjusted Gross Income (MAGI).
However, there are exceptions. Certain individuals, such as those with disabilities, over the age of 65, or enrolled in specific programs like breast and cervical cancer treatment, may qualify even if they don’t meet the MAGI income requirements.
Reasons You Might Face A Medicaid Denial
Even if you meet the basic eligibility criteria for Medicaid, your application can still be denied for various reasons. You will typically receive a Medical denial letter, which will typically include the reason why you’ve been denied. Understanding these reasons can help you determine your next steps and potentially address any issues that led to the denial. Below listed are the most common reasons of a Medicaid denial:
Income or Assets Exceeding Medicaid Limits:If your income exceeds the state-specific income limits, you may be ineligible. You can look at the state by state eligibility criteria to determine whether you qualify or not. But if you think that you are incorrectly denied, you can always first confirm the limits by your state, understand how medicaid actually counts your income and then you may at any time request a reversal. It is always best to discuss your case with a certified Medicaid planning professional.
You can also file a formal appeal to determine the actual cause if you think you are wrongfully denied.
Medicaid’s Look-Back Period Violation: This is another common denial factor. It is basically a penalty period. Medicaid often has a look-back period, typically five years, during which asset transfers are scrutinized. Any assets transferred below fair market value during this period may result in a penalty period of ineligibility.
- Trusts: Placing assets in trusts may also trigger a penalty period if the trust can be accessed by the applicant.
- Spousal Impoverishment: In some cases, spouses may be able to transfer assets to each other without incurring a penalty, but specific rules apply.
Insufficient Medical Needs: In some conditions, even if you have a qualifying condition, your medical needs may not be severe enough to meet Medicaid’s eligibility requirements.
If you believe your denial was unjustified, It’s important that you understand your state’s appeal process and deadlines.
The Appeal Process
When you receive a Medicaid denial, and you feel that your side of the story has not been heard, understanding the appeal process is crucial. Our team is committed to advocating for your oral health and ensuring you receive the necessary orthodontic care. It is understandable that insurance denials can be frustrating and stressful, so we’ll work closely with you throughout the appeal process.
We’ll handle all the paperwork and communication with the insurance company on your behalf, while also guiding you through each step of the appeal so you understand the process and feel empowered. Our goal is to help you achieve the smile you deserve, and we won’t give up until we’ve exhausted all available options.
Here’s a breakdown of the general steps involved:
1. Review the Denial Notice:
- Carefully read the notice to understand the reasons for the denial.
- Pay attention to the deadline for filing an appeal.
2. Gather Supporting Documentation:
- Collect any additional documents that may strengthen your case.
- This might include medical records, financial statements, or other relevant information.
3. Submit a Written Appeal:
- Prepare a clear and concise appeal letter.
- Explain the reasons why you believe the denial was incorrect.
- Include any supporting documentation.
- Ensure you submit the appeal within the specified deadline.
4. Attend the Hearing:
- If a hearing is scheduled, be prepared to present your case.
- Gather any necessary evidence and witnesses.
- Follow the guidelines provided by the Medicaid agency regarding the hearing process.
5. Await the Decision:
- After the hearing, you will receive a written notice of the decision.
- If the appeal is unsuccessful, you may have the option to further appeal the decision.
- If the appeal is successful, you will be enrolled in Medicaid and may be eligible for retroactive coverage.
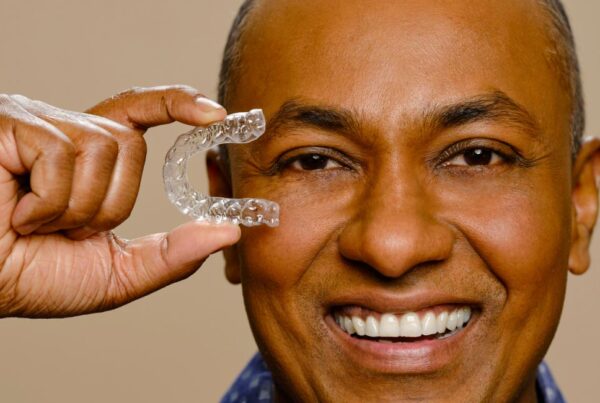
Can You Still Get Braces If You Don’t Have Insurance?
Even if you’ve been denied Medicaid coverage, achieving a beautiful smile is still possible. At Orthodontic Expert, we understand that orthodontic treatment can be a significant investment, which is why we offer affordable payment plans starting at just $195 per month. This flexible option allows you to get the braces you need without breaking the bank.

To qualify for this offer, you’ll need to provide proof of a Medicaid denial. The first payment is due upon signing the contract, and you’ll be committed to a minimum of 24 monthly payments or until treatment is complete. Please note that this offer is applicable only for traditional braces and doesn’t apply to patients who are already enrolled in an active orthodontic payment plan.
Don’t Let A State Insurance Denial Hold You Back
Even if you’ve been denied Medicaid coverage, achieving a beautiful smile is still possible. At Orthodontic Expert, we offer affordable orthodontic treatment options to suit your needs and budget. Our flexible payment plans, starting at just $195 per month, make braces accessible to a wider range of individuals.
Don’t let a Medicaid denial hold you back. Schedule a no-cost consultation today to learn more about our orthodontic services and explore the payment options that best fit your circumstances. Our team of experienced orthodontists is dedicated to providing you with the highest quality care and a smile you’ll love.